The skin on our hands is exposed to a wide range of environmental stressors, including allergens, irritants, frequent washing, and temperature extremes. As a result, chronic skin conditions like psoriasis and eczema often manifest in this area. These conditions can significantly impact daily life—affecting both physical comfort and self-esteem.
What is Psoriasis?
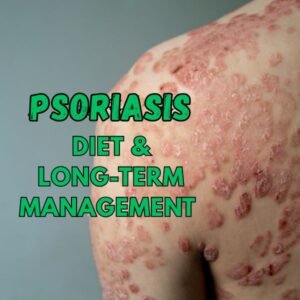
Psoriasis is a chronic autoimmune skin disease characterized by an overproduction of skin cells. This rapid cell turnover causes red, scaly patches that may crack or bleed. It is non-contagious and tends to cycle through flares and periods of remission.
It is primarily caused by an immune system dysfunction where T-cells mistakenly attack healthy skin cells. This leads to inflammation and excessive skin cell growth. While the exact cause remains unknown, genetic and environmental factors are known to contribute.
Types of Psoriasis that Affect Hands
- Plaque Psoriasis: Most common, appears as raised red patches covered with silvery-white scales.
- Palmoplantar Psoriasis: Specifically affects the palms and soles, often causing painful fissures and thick plaques.
- Pustular Psoriasis: Manifests as white pustules surrounded by red skin, frequently on the palms.
Common Triggers of Psoriasis
- Stress and anxiety
- Cold, dry weather
- Skin injuries (Koebner phenomenon)
- Infections, especially streptococcal
- Certain medications (e.g., beta-blockers, lithium)
- Alcohol and smoking
What is Eczema?
Eczema, or atopic dermatitis, is a chronic inflammatory skin condition marked by dry, itchy, and inflamed skin. It often develops in childhood but can occur at any age. Like psoriasis, eczema is not contagious and tends to flare periodically.
Eczema is believed to result from a combination of genetic predisposition and environmental factors. A compromised skin barrier allows moisture to escape and irritants to penetrate, triggering inflammation. It’s often associated with other allergic conditions like asthma and hay fever.
Types of Eczema that Affect Hands
- Irritant Contact Dermatitis: Caused by frequent hand washing or exposure to harsh chemicals.
- Allergic Contact Dermatitis: Triggered by allergens like nickel, latex, or fragrances.
- Dyshidrotic Eczema: Characterized by small, itchy blisters on the sides of the fingers and palms.
Common Triggers of Eczema
- Soaps and detergents
- Allergens (e.g., pet dander, pollen)
- Stress
- Heat and sweating
- Hormonal changes
- Certain foods (in some individuals)
Symptoms Comparison: Psoriasis vs Eczema
| Category | Psoriasis | Eczema |
|---|---|---|
| Appearance of Skin Lesions | Thick, raised plaques with silvery-white scales | Red, inflamed patches with possible oozing or crusting |
| Location on Hands and Fingers | Palms, knuckles, back of hands; well-defined borders | Fingers, between fingers, wrist area; more diffuse |
| Itching vs Pain | Mild to moderate itching; often painful or burning | Intense itching; scratching may lead to infection |
| Onset and Duration | Develops slowly; chronic with flare-ups | Can appear suddenly; fluctuates with triggers |
| Genetic & Environmental Factors | Strongly linked to immune system genes; triggered by stress, infections, climate | Involves skin barrier genes (e.g., filaggrin); triggered by allergens and irritants |
| Age & Demographics | Can occur at any age; most common between 15–35; affects both sexes equally | Often begins in childhood; more common in individuals with family allergy history |
| Underlying Immune Mechanism | Autoimmune—immune system attacks healthy skin cells | Overactive immune response to allergens or irritants |
Diagnosing Psoriasis and Eczema on Hands
Dermatological Examination
A dermatologist will typically start with a visual inspection of the affected skin. They’ll examine the location, shape, and nature of the lesions. Psoriasis often presents as sharply demarcated plaques, while eczema tends to have more diffuse redness and swelling.
Skin Biopsy and Lab Tests
In cases where visual diagnosis is inconclusive, a skin biopsy may be performed. This involves taking a small sample of skin for microscopic analysis to distinguish between psoriasis and eczema at the cellular level.
Importance of Medical History
A detailed medical history, including family background, history of allergies, triggers, and the evolution of symptoms, can offer crucial clues. Understanding whether a patient also has conditions like asthma or autoimmune diseases helps tailor the diagnosis and treatment plan.
When to See a Dermatologist
While mild flare-ups may be managed at home, it’s essential to consult a dermatologist if:
- Symptoms persist or worsen despite using over-the-counter treatments
- The skin becomes infected (e.g., oozing, yellow crusts)
- Cracks, bleeding, or extreme dryness affect your ability to use your hands
- There’s uncertainty about the diagnosis
- Quality of life is negatively impacted
Importance of Early Diagnosis
Early and accurate diagnosis can prevent complications such as scarring, infections, or joint involvement (in the case of psoriatic arthritis). A dermatologist can help create a personalized treatment plan that reduces symptoms, lengthens remission periods, and enhances daily functioning.
Myths and Misconceptions
Common Misunderstandings about Psoriasis and Eczema
- “Psoriasis and eczema are contagious.”
False. Neither condition is infectious or can be spread through skin contact. - “Only children get eczema.”
Incorrect. While eczema often starts in childhood, adults can also develop or retain the condition. - “Poor hygiene causes skin problems.”
Not true. In fact, over-washing hands with harsh soaps can trigger or worsen symptoms.
Clarifying Treatment Expectations
- “There’s a cure.”
Unfortunately, there’s no definitive cure for either condition. Treatments aim to manage and reduce symptoms. - “Natural remedies are always better.”
While some natural solutions may help, they are not universally effective and may even irritate sensitive skin. Always consult a healthcare provider before trying home remedies. - “Steroid creams are dangerous.”
When used as prescribed, topical steroids are safe and effective. Problems generally arise from misuse or overuse without medical guidance.