I see many people in my clinic who are frustrated by psoriasis – the itch, the flare-ups, the uncertainty. I want to share what I’ve learned over the years: what helps, what doesn’t, and how to manage psoriasis in ways you can live with – not just treat.
I’ll explain things in simple language, share real experiences, and help you understand what science says now (because “what works” evolves over time). If anything feels too medical, just let me know – I’m happy to clarify.
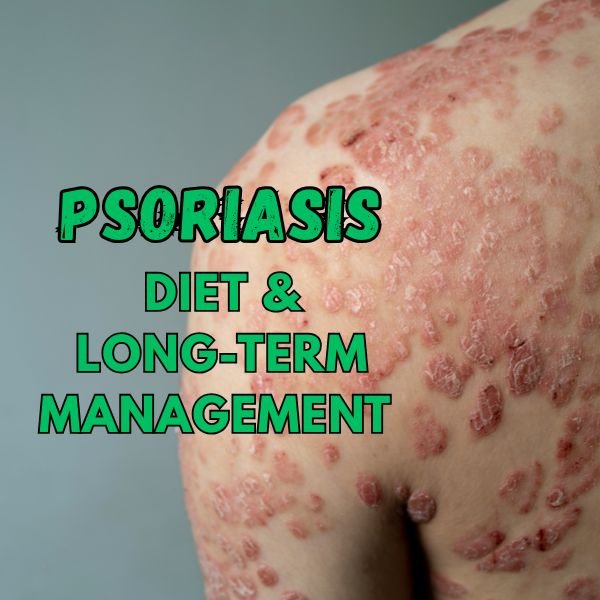
What is Psoriasis – My Experience & The Basics
- Psoriasis is a chronic (long-lasting) skin condition. It is an immune system reaction: your body’s immune cells get overactive and speed up skin cell growth. This leads to thick, red patches of skin with silvery scales.
- It tends to come in cycles: times when symptoms are bad (“flare-ups”) and times when things are better (“remission”).
- Genetic factors matter (if someone in your family has it), but triggers also play a key role — things like stress, illness, skin injury, certain medicines.
I remember a young patient who said her psoriasis always worsened after exams because of stress and poor sleep. Once she started paying attention to sleep and managing stress, her flare-ups reduced significantly.
Can Psoriasis Be Cured Permanently?
Short answer: No proven “permanent cure” yet, but yes, long-lasting control is possible.
Here’s what I tell patients:
- “Cure” implies the disease goes away forever and never returns. We don’t have that yet for psoriasis.
- But “remission” — long periods with very mild or no symptoms — is possible with good treatment + lifestyle + avoiding triggers.
- Some people may remain symptom-free for months or even years, if they manage well. But there is always a chance of flare-ups.
So, think of management rather than cure. My goal as a dermatologist is to help you get into remission, reduce flare-ups, improve your quality of life.
Diet Plan for Clear Skin: What Helps, What to Try
Based on recent research, and what I’ve seen in patients, what you eat can influence psoriasis — not usually as a single cure, but as an important helper.
Here are guidelines I give:
Foods / Eating Patterns That Help
- Plant-rich, low saturated-fat diets1
- Diets with lots of vegetables, fruits, whole grains, legumes, nuts, lean proteins are linked to less severe psoriasis.
- For example, a Mediterranean-style diet (olive oil, fish, vegetables, few processed foods) shows promise.
- Weight control
- If someone is overweight or obese, even modest weight loss tends to reduce severity of psoriasis.
- I’ve had patients who lost just 5-10% of body weight see noticeable improvement in their skin.
- Omega-3 fatty acids
- Found in fatty fish (salmon, mackerel), flaxseed, walnuts. These help reduce inflammation.
- High fibre & low sugar, low processed food
- Less refined sugars, fewer highly processed items is better. Fibre (whole grains, legumes, vegetables) seems to correlate with less severity.
Foods / Things to Avoid or Limit
- High saturated fats and trans fats (e.g. in fatty red meat, deep fried, processed snacks).
- Excess sugar, sugary desserts, sugary drinks.
- Possibly dairy, gluten (if tested positive for gluten sensitivity) may worsen psoriasis in some people. Not everyone reacts the same.
- Alcohol can be a trigger in many individuals.
What a Sample Day Might Look Like
Here’s what I often suggest patients try, especially during flare-ups:
| Meal | Example |
|---|---|
| Breakfast | Oatmeal with chopped nuts + berries; or vegetable omelet with olive oil; herbal tea or water |
| Lunch | Grilled fish or legumes (beans/lentils), big mixed salad (varied veggies), whole grain bread / brown rice |
| Snack | Mixed nuts, fruit, perhaps a small yogurt (if dairy tolerated) |
| Dinner | Roasted or steamed vegetables, lean protein (chicken, fish, tofu), quinoa or millet |
| Hydration & Extras | Plenty of water; limit sugary drinks; gentle herbal teas; avoid overeating late at night |
It’s important to try changes gradually – don’t overhaul everything overnight. Keep a journal: what you eat, how your skin responds. That helps identify your individual triggers.
Treating Psoriasis Without Steroids
Many people ask me: “Are steroids bad?” “Can I treat without them?” I understand – steroids can help, but they come with side effects. Here’s what I share:
Why people want to avoid steroids
- Overuse of topical steroids can thin the skin, cause stretch marks, discoloration, and sometimes dependency.2
- For long-term use, minimizing steroid exposure is safer.
Non-steroid options (topical and systemic)
- Topical treatments
- Vitamin D analogues (help slow skin cell growth).
- Coal tar, salicylic acid to remove scales.
- Emollients / moisturizers to reduce dryness & itching.
- Phototherapy
- Controlled UVB light exposure under medical supervision. Helps many patients greatly.
- Systemic non-steroid treatments (for moderate to severe cases)
- Biologic agents (target specific immune pathways), small molecule drugs, etc. These are prescribed when topical + lifestyle + diet are not enough.
- Natural / Complementary methods
- Stress reduction (mindfulness, deep breathing, yoga).
- Proper skin care: gentle cleansers, avoid harsh soaps; avoid skin trauma.
- Lifestyle: good sleep, regular exercise.
In my practice, I’ve seen that patients who combine non-steroid medical treatments with diet & lifestyle tend to achieve longer remission.
Does Coconut Oil Help Psoriasis?
You may have heard “coconut oil is good for psoriasis.” Let me tell you what I understand from studies and from what I see in clinic.
What it can do
- Moisturizing: Coconut oil is a good emollient. It helps keep skin hydrated, which is very important. Dry, cracked skin often flares more.
- Anti-inflammatory and antimicrobial properties: Virgin coconut oil (cold-pressed) has components that may reduce inflammation and fight organisms that can worsen skin irritation.
What it doesn’t do / limitations
- It is not a cure. Even if it helps with scaling, itching, and appearance, it does not change the underlying immune overactivity. So expect it to help as a support, not to completely stop psoriasis by itself.
- Some studies show that applying emollients (including coconut oil) before certain phototherapy treatments might interfere with the light therapy, because oils can absorb UV. So we must use these carefully.3
- Allergy or irritation: a few people are sensitive; always test on a small patch first.
How I suggest patients use it
- Use virgin / unrefined coconut oil (if possible) on patches that are dry or scaling.
- Apply after bathing, when skin is slightly damp, to lock in moisture.
- Use it alongside other treatments — moisturizers, prescribed doctors’ topicals — not instead.
- Monitor: if you see irritation, stop or reduce frequency.
Putting It All Together: Realistic Expectations & Long-Term Strategy
From many years treating patients, here’s what I tell them to expect and aim for:
- Control, not perfection. We often can’t erase all patches permanently, but we can reduce severity, reduce flare frequency, make life comfortable.
- Be patient. Lifestyle/diet changes take time to show effect (weeks to months). Don’t expect overnight remission.
- Personalization: what works for one person may not work for another. Keep track: which foods seem to trigger flare-ups for you.
- Work with a dermatologist: combine medicines/lifestyle/diet. Sometimes trying different therapies if something isn’t working.
- Watch for comorbidities: psoriasis is linked with arthritis, heart disease, metabolic issues. So your diet, weight, general health matter not just for your skin.
Frequently Asked Questions
Q. Is psoriasis contagious?
A. No — you cannot catch psoriasis from someone else. It’s not an infection.
Q. Will children outgrow it?
A. Sometimes children see improvement as they grow, but in many cases psoriasis persists or recurs.
Q. How will I know what foods trigger my psoriasis?
A. Keeping a food skin-response journal helps. An elimination diet (removing suspect items, then reintroducing) under supervision can help.
Q. When should I see a doctor?
A. If flare-ups get bad, cover large areas, are causing pain, interfering with sleep / daily life, or if treatments aren’t helping. Also if you notice joint pain (psoriatic arthritis).
Conclusion
I believe — from both science and my clinic — that while psoriasis cannot yet be permanently cured, it absolutely can be managed well. Diet, natural care (like coconut oil), avoiding triggers, non-steroid treatments, and good medical supervision together give you the best chance of long remission and clearer skin.
If I were you, I’d start by making small, doable changes: improve diet a bit (more plants, less processed food), keep skin well moisturized, use gentle treatments, and monitor how your skin responds. Over time, you’ll discover your combination that works best.
If you like, I can also prepare a version of this blog geared specifically for an Indian audience (foods available locally, recipes, etc.). Would you prefer that?