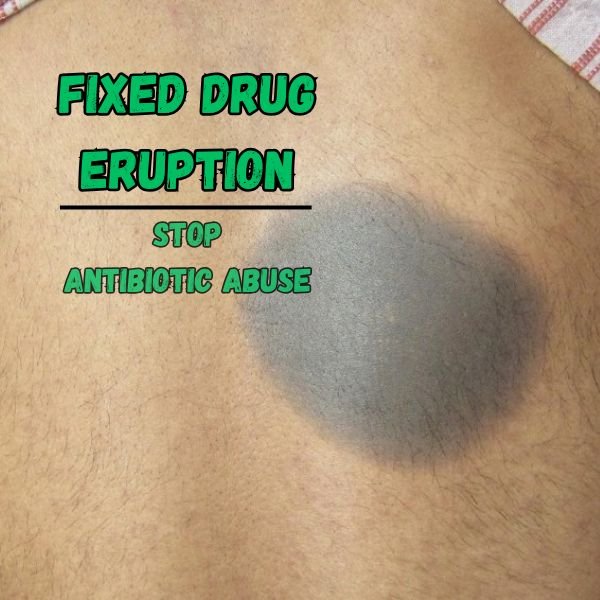
Imagine this: you feel unwell with diarrhea, take an antibiotic without much thought, and then days later a painful, dark patch appears on your skin. The patch heals slowly, but the mark remains—and the next time you take the same antibiotic, the exact same patch comes back, sometimes worse. This is not just coincidence. It’s a condition known as Fixed Drug Eruption (FDE), a skin reaction that can be triggered by certain medicines, especially antibiotics. As a dermatologist, I often see patients struggling with these marks, which could have been avoided if antibiotics had been used more carefully.
The truth is, not every case of diarrhea needs antibiotics, and sometimes taking them does more harm than good. Let’s break this down in simple terms.
What Is a Fixed Drug Eruption?
A Fixed Drug Eruption is a skin reaction caused by a medicine. Unlike a rash that spreads randomly, FDE has a very unique feature: it always reappears in the same spot each time you take the same medicine. It usually looks like a round or oval patch that starts red or purple, can form a blister, and then heals with a dark mark. These marks may fade slowly, but often they leave a permanent stain on the skin.1
Common areas where these patches appear include the lips, face, hands, legs, genitals, or trunk. They can be uncomfortable, itchy, or even painful. The reaction usually starts within hours or a day of taking the medicine again, which makes the link quite obvious once you know what to look for.
The reason behind FDE is your body’s immune memory. Once your immune system “decides” that a medicine is harmful, it keeps a record of it. The next time the same drug enters your body, your skin reacts instantly in the exact same place. It’s like a warning sign your skin refuses to forget.
Why Antibiotics Often Trigger Fixed Drug Eruptions
While many different drugs can cause FDE, antibiotics are among the most common culprits, according to the decreasing order of number of reports:2
- Norfloxacin
- Metronidazole
- Paracetamol/ Diclofenac/ Naproxen
- Cotrimoxazole (TMP-SMX)
- Ibuprofen
- Ciprofloxacin / Ofloxacin Levofloxacin
- Ampicillin
- Doxycycline
- Fluconazole
- Aspirin
- Carbamazepine
Fluoroquinolones, especially norfloxacin, are often top offenders in FDE cases.
Nitroimidazoles (e.g., metronidazole, tinidazole) and NSAIDs (like ibuprofen, diclofenac, naproxen) also rank high, reflecting frequent prescription patterns.
Regional prescribing habits significantly affect FDE prevalence—e.g., cotrimoxazole was the leading cause in some regions but not others.
The problem is not just that antibiotics can cause these reactions, but that they are often taken when they are not even needed. Every unnecessary dose exposes you to the risk of a drug eruption.
The Truth About Diarrhea and Antibiotics
Diarrhea is one of the most common reasons people reach for antibiotics, but here’s the fact: most cases of diarrhea do not require them. In many situations, diarrhea is caused by viruses or by eating contaminated food or water. These cases usually resolve on their own with rest, hydration, and a light diet.
When antibiotics are used carelessly for diarrhea, three harmful things happen.
First, antibiotics disturb the natural balance of bacteria in your gut, which can actually make your digestion worse and increase the risk of future stomach problems.
Second, overuse of antibiotics contributes to antibiotic resistance, which means that when you truly need these medicines in the future, they may no longer work.
Third, and often ignored, is the fact that antibiotics can trigger Fixed Drug Eruptions, leaving behind painful patches and dark stains on your skin that can last for months.
A Real-Life Example
I once treated a patient who developed a dark patch on the lip every time they took antibiotics for diarrhea. At first, they thought it was just a coincidence. But after the same thing happened multiple times, it became clear this was a fixed drug eruption. The antibiotic, meant to treat the stomach upset, was actually causing a stubborn skin reaction that was more troubling than the diarrhea itself.
Once we stopped the unnecessary antibiotic use and managed the diarrhea with hydration and dietary care, the patches stopped recurring. The patient was relieved, though the dark mark on the lip remained as a reminder of how unnecessary medication can leave lasting scars.
How Dermatologists Promote Safer Choices
Dermatologists, along with other doctors, play an important role in guiding patients away from unnecessary antibiotic use. The first step is careful assessment. If a patient comes in with diarrhea, the doctor will look for warning signs such as high fever, blood in the stool, or severe dehydration.
These are the situations where further tests and sometimes antibiotics may be needed. But for most mild cases, the treatment is supportive—hydration, oral rehydration salts, rest, and a simple diet until the stomach settles.
Another important part of our job is education. Patients need to understand that antibiotics are not cure-all medicines. They can save lives when used correctly, but they can also cause harm when used carelessly. By explaining the risks of side effects like fixed drug eruption, patients are empowered to make better choices.
What to Do If You Suspect Fixed Drug Eruption
If you notice that a skin patch appears every time you take a certain antibiotic or medicine, stop taking it immediately and see a dermatologist. The doctor will confirm if it is a fixed drug eruption and help you manage the reaction.
In most cases, stopping the drug is enough, and the skin will slowly heal. To ease symptoms, doctors may prescribe soothing creams or medicines to reduce itching and inflammation. However, the most important step is prevention. Always remember which drug caused the reaction, keep a note of it, and inform every doctor you visit so you don’t get prescribed the same medicine again.
Conclusion
Fixed Drug Eruption is a skin condition that acts like your body’s alarm system against certain medicines, especially antibiotics. Overusing antibiotics for something as common as diarrhea is risky, unnecessary, and often harmful. Not only can it damage your gut and increase resistance, but it can also leave visible scars on your skin.
The next time you or someone you know has diarrhea, remember this: most cases get better without antibiotics. Save antibiotics for the times when they are truly needed, and listen to your skin—it often knows when something isn’t right. By making careful choices, you protect not only your stomach but also your skin, your health, and your future.